As healthcare providers, we often spend more time focusing on the cardiometabolic effects of obesity and forget about the psychologic aspects. It should be obvious to anyone in America that there is a huge prejudice against the overweight/obese in society. This isn’t surprising, but you may be surprised to find this same sort of prejudice in the clinical setting – a place where patients expect their clinicians to treat them with empathy and respect.
For example, primary care providers were asked about their attitudes on the obese (defined as BMI > 40 in one sample and BMI > 30 in the other to see differences in attitude related to BMI). What did they find? [1]
More than 50% of physicians viewed obese patients as awkward, unattractive, ugly, and noncompliant…Primary care physicians view obesity as largely a behavioral problem and share our broader society’s negative stereotypes about the personal attributes of obese persons.
Surprisingly, we found few differences based on physician characteristics (including BMI and gender) or how obesity was defined in the survey. Among those that were detected, the mean differences were very small, raising doubts about their clinical significance.
This perspective may even be more prevalent in younger primary care providers: [2]
We found higher prevalence of negative attitudes toward obese patients than reported by others. For example, almost 80% of our respondents reported that patients frequently or almost always lacked discipline, and 52% felt patients lacked motivation to lose weight.
The high prevalence of negative attitudes may hinder primary care physicians from discussing weight loss with extremely obese patients. It was interesting that older age and higher patient volume were independently associated with less negative attitudes. Perhaps, physicians with more experience or who are more successful develop a “tolerance” toward patients with extreme obesity.
There was a high prevalence of negative attitudes, particularly in younger physicians and those with lower patient volume. Increased knowledge of weight-loss diets was associated with less dislike in discussing weight loss (P < 0.0001), less frustration (P = 0.0001), less belief that treatment is often ineffective (P < 0.0001), and less pessimism about patient success (P = 0.0002)…further research is needed to determine if interventions to increase knowledge of physicians will lead to less negative attitudes toward weight loss and extremely obese patients.
It’s hard to say why some clinicians may feel this way towards the obese. Do the negative attitudes occur because of societal beliefs? Or do they occur due to frustration at not seeing weight loss from patients after intervention? I would argue it’s a combination of both with one belief reinforcing the other. However, is the difficultly in helping patients lose weight really a result of low “will power” or “discipline?” Perhaps providers have the wrong beliefs about causes of obesity in the first place – which influences the interventions they are likely to tell their patients. From the first study on primary care provider beliefs:
Physical inactivity (mean rating of 4.3) was rated significantly more important than any other cause of obesity (p < 0.0009). Two other behavioral factors—overeating and a high-fat diet— received the next highest mean ratings (3.9 and 3.8, respectively; 3, moderately important; 4, very important; 5, extremely important).
So primary care providers seemed to rate physical inactivity as the leading cause of weight gain in obesity. It definitely is true that exercise can help a person lose weight, but exercises’ effect on weight loss is more dramatized than reality. In Identifying the difference between exercise + diet versus diet alone in randomized control trials by the Cochrane Collaboration, the difference with the addition of exercise was: [3]
In the group exercise plus diet versus diet alone fourteen trials involving 1049 participants included data regarding weight loss that were suitable for meta-analysis. Participants in both groups lost weight across trials. The pooled effect for interventions with a follow-up between 3 and 12 months was a reduction in weight of 1.1 kg (95% confidence interval (CI), 0.6 to 1.5) in the exercise and diet group compared with the diet alone group.
So the difference these RCTs found with the addition of exercise + diet versus diet alone was an average of 2.4 lbs lost in favor of exercise with diet. Again, the addition of exercise does help with more weight loss but hardly the amounts that all those late night exercise gadget infomercials portray. This is not to say that one shouldn’t bother with exercise if they are already eating right – exercise has other obvious benefits.
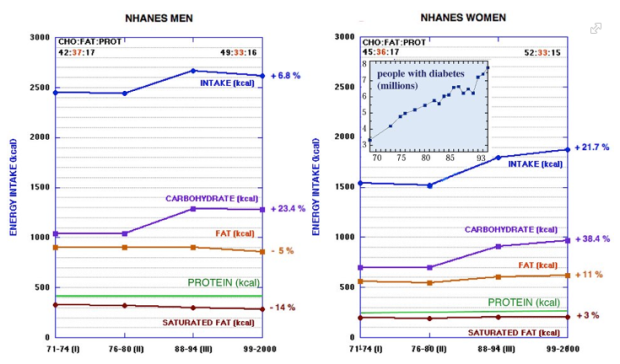
Going back to the study on primary care provider attitudes on obesity, you’ll notice that the next two highest rated beliefs providers have on causes of obesity are: overeating and a high fat diet. One of these points is not supported by the literature. If you look at the National Health and Nutrition Examination Survey (NHANES) from the CDC you’ll see this:
It is definitely true that both Men and Women are eating more calories since the 80’s…but is it from a high fat diet? Men have actually decreased their total fat and saturated fat calories while women have increased both. However, both men and women have increased their dietary carbohydrate by vast margins at + 23.4% and + 38.4% respectively! If one is to believe a high fat diet is one of the independent causes of obesity, how can they discount the increase in carbohydrate as a factor as well?
Additionally, the increase in carbohydrate consumption likely contributes to the increases in overeating/calories. This requires a paradigm shift from viewing a calorie is a calorie and focusing on the hormonal, physiologic and psychologic effects that macronutrients have on the body and mind. By doing so, we can see that a patient’s inability to lose weight has nothing to do with a lack of discipline, laziness or willpower to reduce/count calories. Instead, it may just be that they’ve been receiving the wrong advice in the first place.
BTW, before this post ends, it should also be pointed out that negative attitudes/beliefs to the obese applies to clinicians from the patient’s perspective as well. From a study last month: [4]
Respondents reported more mistrust of physicians who are overweight or obese, were less inclined to follow their medical advice, and were more likely to change providers if the physician was perceived to be overweight or obese, compared to normal-weight physicians who elicited significantly more favorable reactions.
These weight biases remained present regardless of participants’ own body weight. Stronger weight bias led to higher trust, more compassion, more inclination to follow advice, and less inclination to change doctors when the physician was presented as normal weight. In contrast, stronger weight bias led to less trust, less compassion, less inclination to follow advice and higher inclination to change doctors when the physician was presented as obese.
This study suggests that providers perceived to be overweight or obese may be vulnerable to biased attitudes from patients, and that providers’ excess weight may negatively affect patients’ perceptions of their credibility, level of trust and inclination to follow medical advice.
At the end of the day, after all this talk of health and weight, let’s just treat individuals as individuals irrespective of their weight.
Summary: The prejudice that the obese face in society is very prevalent, but this negative attitude may also be present in the healthcare setting from clinicians. It’s hard to say if these attitudes from clinicians originated with the same prejudice from society in general, or if they are from clinicians developing negative attitudes due to lack of success in treating their obese patients. Interestingly enough, patients have negative attitudes about their providers if the provider is obese. In the end, let’s just get respect one another whether a person is obese or not.
1) Foster, G. D., Wadden, T. A., Makris, A. P., Davidson, D., Sanderson, R. S., Allison, D. B., & Kessler, A. (2003). Primary care physicians’ attitudes about obesity and its treatment. Obesity Research, 11(10), 1168-1177.
2) Ferrante, J. M., Piasecki, A. K., Ohman-Strickland, P. A., & Crabtree, B. F. (2009). Family physicians’ practices and attitudes regarding care of extremely obese patients. Obesity, 17(9), 1710-1716.
3) Shaw, K., Gennat, H., O’Rourke, P., & Del Mar, C. (2006). Exercise for overweight or obesity. Cochrane Database Syst Rev, 4.
4) Puhl, R. M., Gold, J. A., Luedicke, J., & DePierre, J. A. (2013). The effect of physicians’ body weight on patient attitudes: implications for physician selection, trust and adherence to medical advice. International Journal of Obesity.